2019 New Year Resolutions 2: Confirming authorizations and referrals
During certain times of the year -- January and July, for example –– many of your patients switch to a new health plan and staying ahead of authorization and referral requests can be a double-edged sword. It’s best practice to request an authorization or referral well ahead of the patient’s scheduled service. But if the patient changes health plans during the period between the request and the service, you might end up with a denied claim.
During these busy open enrollment seasons, it’s important to double-check that your patient is still with the health plan you submitted the request to.
Check referrals and authorizations online
Most health plans will let you check and create referral and authorization requests online in their provider portal. In NHPNet, you can lookup authorizations and referrals by Member ID or by Authorization/Referral ID. You can also click on the corresponding link to view all authorizations and referrals for your practice.
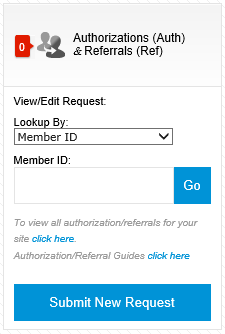
If the appropriate authorization or referrals are not in place, press the “Submit New Request” button to get started. Click Here for some useful instructions on how to submit authorizations and referrals.
Don’t get stuck with a denied claim
Remember:
- Prior authorization requirements vary from plan to plan, so check with the new health plan to understand their continuity of care policy
- If a date of service spans across two different insurance plans, you might need to obtain two different authorizations
- If a patient switches from a PPO to an HMO they will need a referral and the patient will need to coordinate that with your practice
If you do send a request to the wrong health plan, make sure you send a corrected claim ASAP and know each health plans filing limits. For example, the NHP filing limit is generally 90 days unless otherwise indicated in your contract.
Appeals and denials can cost you a lot in time and effort. Ensuring that the appropriate authorizations and referrals are in place before a claim goes out the door can be a much-needed step during a very busy time.
Did you miss Part I of this series, Confirming Eligibility? No problem! You can read it here.
